A New Paradigm for Adults with Serious Illness and Complex Care Needs
Working Together to Build a Person Driven, Community Centered, Intergrated Care Network

The Honoring Choices MA Person Driven, Community Centered Intergrated Care Network Advisory Group's mission is to shift from the current hierarchical care paradigm to an improved person driven, team based, community centered, integrated care network for adults living with chronic and serious illness and complex care needs.
Our collective goal is to work in shared leadership with healthcare and community stakeholders and elevate the voices and knowledge of consumers and community coalitions, to inform and guide an improved infrastructure. Together we can ensure individuals with chronic and serious illness and complex care needs live their best lives and can access timely, equitable care at home and in their community.
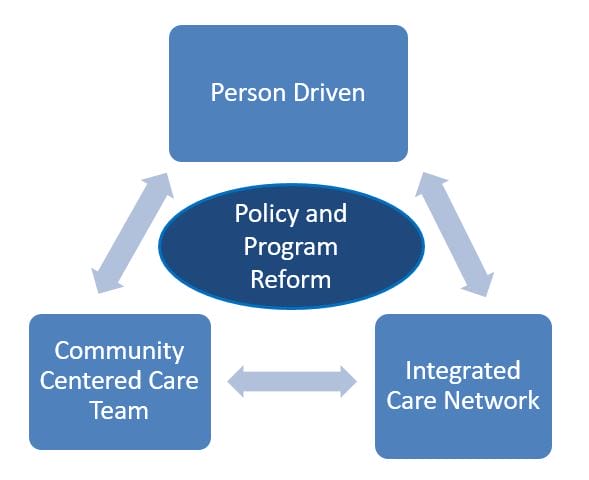
Policy and Program Reform that Advances Health Equity
Building a New Paradiym: Mission and Goals
Policy and program reform that advances health equity is at the heart of a new paradigm to build an improved-
1. Person Driven to recognize the right of every individual to direct their health care choices, and work in partnership with their health care providers for good care today and over their lifetime;
2. Community Centered, Interprofessional Care Team approach to support an inclusive, well prepared, culturally competent, valued workforce to address the community need;
3. Integrated, collaborative care network that disrupts root causes of racial and health inequities, addresses social drivers of health, and builds new pathways to access timely quality care at home and in the community.
Getting Started: Three Workgroups Set Actionable Objectives
The Advisory Group members began to build the collaborative infrastructure within three workgroups. Each workgroup defined a common vision and a set of recommendations to achieve the goals through immediate actionable objectives. As our collaboration and workgroups grow, we will refine the goals and expand the objectives to build an inclusive integrated cross continuum care network.
Workgroup 1: Person Driven and Community Centered Program Reform

Convenes a Person Driven Community-Based Palliative Care in MA Workgroup.
Access to affordable, community based, equitable Palliative Care is a game changer for individuals with serious illness. To work towards that objective for MA adults and families, this workgroup is hosting webinars for a unique learning opportunity and an exchange of ideas with interprofessional care team members and consumers. All are welcome to join the conversation and explore resources.
Envisioning Person Driven Community-based Palliative Care in MA
Session 1, September 28, 2024
Summary: Key elements and lessons learned in delivering community-based palliative care services to a diverse, inclusive Medicaid population. Virtual event for all Interprofessional Care Team Members
Guest Speakers: Dr. Anne Kinderman, Loren Porig, Kathleen Kerr, Transforming Care Partners. Consultants on California Medicaid Managed Care Palliative Care mandate
Resources for on-going exploration and discussion:
Session 2, January 28, 2025
Resources
- Hospice & Palliative Care Fed of MA- Palliative Care Directory
- The Case for Community Based Palliative Care, Center to Advance Palliative Care (CAPC)
- Session 2 Guest Speaker Presentation...
Vision Statement
The vision is for the people of Massachusetts living with a serious illness to access an equitable, person driven, team based, community centered Palliative Care across home and community settings.
As home and community palliative care champions, consumers, and providers, we advocate equity in a Massachusetts Medicaid Benefit that represents the voice and needs of all individuals with serious illness, which includes underrepresented, uninsured, and historically marginalized individuals.
The role of our highly collaborative workgroup is to elevate the person, family and community voices to determine what individuals actually need in a Massachusetts community palliative care benefit.
Taking the necessary steps to craft a person driven, community centered benefit, will help us know how to increase access to palliative care in medical clinics, care facilities, and in home and community settings. It will intentionally address racial and health inequities to help ensure all individuals living with serious illness receive responsive, proactive and timely care that prevents crisis and improves quality of life for individuals and families.
Working together we can help ensure the needs of people with serious illness are served in an impactful and meaningful way by a sustainable and equitable community palliative care medicaid benefit.
Recommendations
Drawing from successful evidenced based models, we recommend a Massachusetts Community Palliative Care mandate that is-
- Person driven, where individuals and their advocates inform and guide the crafting of the trusted, inclusive, Medicaid benefit, which errs on the side of expanded clinical eligibility;
- Team based, which requires care delivery by an appropriately trained, culturally and linguistically competent, well-paid, interprofessional care team;
- Home & community centered palliative care services, which collaborates with the health care ecosystem to provide essential supportive services and benefits, and address the structural barriers and social drivers of health that impact access to holistic, proactive and timely care;
- Inclusive of a bundled payment structure to deliver effective longitudinal team based care;
- Focused on improved systems integration, leveraging technology for shared communication and refined interactive workflows to support the coordination of palliative care services.
Workgroup 2: Support a Community Centered Interprofessional Care Team

Goal: Create an inclusive, well-trained, well-paid, home & community workforce that can trigger proactive timely care.
This goal includes educating both the consumer and care teams members with a structured approach to health care planning for early, effective on-going planning conversations.
Vision Statement:
This workgroup is focused on identifying and supporting a well-trained, culturally competent, well paid, home & community based workforce to start early and ongoing planning conversations and deliver holistic, timely care that honors an individual's values, goals and care preferences.
The workgroup will propose updating state and organizational policies and procedures which empower the interprofessional care teams to work at the top of their skill set and license/accreditation and trigger proactive and timely referrals for care and services.
Recommendations:
- Identify an inclusive and diverse spectrum of home and community based interprofessional care team members;
- Provide care teams educational trainings regarding the Health Care Planning Process and Serious Illness Care Communication to home & community workforce across the care continuum. The training will include the Honoring Choices MA Health Care Planning Process and multi-lingual planning tools, Ariadne Labs Serious Illness Conversation Guides and MA Health & Hospital Association Simple Step Campaign;
- Provide consumers with information, tools and programs that are linguistically and culturally appropriate for meaningful conversations with interprofessional care team.
- Propose state, institutional and organization policy change to enable the home & community care teams to work at the top of their skill set and license/accreditation, and trigger upstream proactive and timely referrals for care and services.
Workgroup 3: Build a Collaborative, Integrated Cross-Continuum Care Network

Create a shared leadership model to bring together new and proven program, dismantle barriers and build new pathways.
Vision Statement:
Community and home based stakeholders share leadership and responsibility to build and sustain an integrated, community centered care network for individuals living with serious illness and complex care needs.
The workgroup is proposing policy, program and payment change which adresses the root causes of health inequitites and social driversthat impact health, and aligns care and services across health care and community settings to support a community centered infrastructure.
Recommendations:
- Invite existing and new home & community based programs to come together in a shared leadership and responsibility infrastructure;
- Invite consumers to inform and guide policy and programs to ensure the home & community centered care network actually serves the needs of adults, families and communities;
- Support community coalitions to address local barriers and build new pathways to promote healthy vibrant communities;
Everyone is Welcome. Everyone Benefits!

Join us. Lend your voice and leadership.
Our Advisory Group members, noted below, collaborated for over 18 months to design the shared leadership infrastructure and spearhead the three workgroups to get us underway.
We are now READY to invite all stakeholders and consumers to lend your knowledge and expertise to refine and expand this collective initiative.
Ways to Contribute:
- Please join a workgroup . The time commitment is very manageable as we work on focused achievable objectives.
- We intentionally seek to coordinate with similarly focused organizations and groups to come together on shared goals and responsibilities.
Contact Ellen DiPaola, Honoring Choices MA, edipaola@honoringchoicesmass.com to learn more and offer your feedback.
Many thanks to our dedicated Advisory Group:
- Erin Nahrgang, RN, CCM, Senior Director, Boston Medical Center, ACO Complex Care Management, Population Health.
- Christine McMichael, Executive Director, Hospice & Palliative Care Federation of MA.
- Colleen Pierro, Director of Regulatory and Clinical Affairs, Home Care Alliance.
- Elizabeth Collins, MD, Chief, Palliative Care, retired, Beth Israel Lahey Health.
- Constance Dahlin, MSN, ANP-BC, ACHPN, FPCN, FAAN, Palliative Care Specialist
- Sarah Livermore, PhD; NP, Complex Care Clinician at Tufts Health Plan
- Paula Griswold, Executive Director, MA Coalition for the Prevention of Medical Errors.
- Stephanie Baker, MHA, CPHQ Quality Improvement Manager Healthcentric Advisors.
- Laura Vanderhill, Senior Quality Improvement Specialist, Healthcentric Advisors
- Joanne Calista, Executive Directive, Center for Health Impact, Worcester.
- Dawn Hobill, Quality Manager, Executive Office of Elder Affairs.
- Silvana Kirby, Medical Interpreter Program, Berkshire Area Health Education Center
- Lauren Cramer Finnerty, Pediatric Advance Care team; Boston Children’s Hospital, Dana- Farber.
- Nicole DePace, Nurse Practitioner, Community Palliative and Hospice Care
- Dawn O’Toole MSN, POINT 32 Health Senior Manager, Integrated Medicare Business.
- Kim McCarthy, BS RN CCM CHPN, POINT 32 Health, Integrated Care Management, Nursing.
- Sharon George, CCHW, Boston Medical Center HARP Team, Population Health.
- Loberta Legrand, Community Wellness, Boston Medical Center Complex Care Management
- Regine Thevenin, Director, MA Comprehensive Cancer Health Equity Program, DPH.
- Melanie Steeves, MPH, Director, Comprehensive Cancer Control Program, DPH
- Kate Granigan, MSW, LICSW, COO, LifeCare Advocates; Community Care Management.
- Emily Palmer, Community NP, Palliative and Hospice Care
- Yael L. Tarnish, MD, Yael Tarshish, MD, Medical Director of Palliative Care, Baystate Health.
- Jodi Kashouh MS RN BC CNL, Baystate Health Healthcare Quality Specialist, Transitions to Coordinated Community Care Network
- Ellen DiPaola, JD, President & CEO, Honoring Choices Massachusetts.
Interested in joining a workgroup?
Let us know how to contact you.
"*" indicates required fields